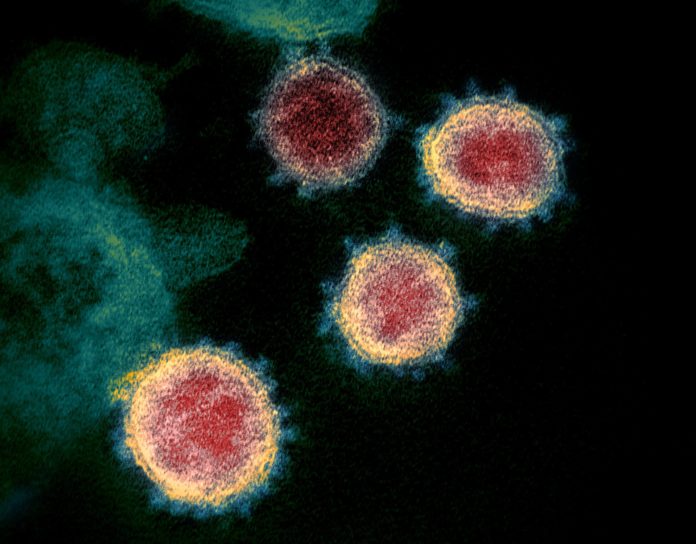
We think of covid-19 as a disease of the respiratory tract. When future generations look back on this pandemic, its iconic symbol will probably be the ventilator. But, although respiratory problems are at the core of the disease, covid-19 has revealed itself to be more than a straightforward viral pneumonia. Doctors around the world — including in the emergency department where we work, at Mount Sinai Hospital, in Manhattan — have learned the hard way that the coronavirus doesn’t confine its ravages to the lungs. covid-19 can push kidneys into failure, send the body’s immune system into catastrophic overdrive, and cause blood clots that impede circulation to the lungs, heart, or brain. It’s a disease of remarkable complexity, which even the most experienced doctors are struggling to understand.
On blogs, podcasts, and #medtwitter, members of the medical community have been trading stories and theories about covid-19’s intricacies. Often, their conversation has followed the methodology of critical-care doctors. Physicians who work in I.C.U.s tend to talk not about symptoms or diseases — chest pain, diabetes — but about organ systems, which can malfunction and interact in complex ways. System by system, a picture of covid-19 is emerging. Clarifying it may mean the difference between life and death for thousands of people in the months to come.
The shortness of breath that’s most characteristic of covid-19 is reasonably well understood. It originates in the gossamer air sacs of the lungs, called alveoli, where blood and air are separated by such thin membranes that oxygen and carbon dioxide can pass into and out of the bloodstream, respectively. Between them, the lungs have somewhere in the neighborhood of six hundred million alveoli. Severe covid-19 causes many of them to either collapse or fill with fluid. The virus attacks the cells lining the alveoli; our overactive immune systems, in trying to fight the virus, may be damaging them as well. The result is that not enough oxygen gets into the blood.
Doctors trying to solve this problem have two basic tools at their disposal: oxygen and pressure. They can give patients concentrated oxygen beyond the usual twenty-one per cent that is found in normal air. Alternatively, using a cpap machine or ventilator, they can create a kind of sustained air pressure within the lungs — “positive end-expiratory pressure,” or peep — which keeps the alveoli open, and thus more receptive to oxygen, at moments when the lungs would ordinarily be emptier of air. (Imagine breathing in and out while leaning through the window of a moving car: that lungs-full-of-air feeling is peep.) Doctors have also been improving oxygenation by “proning” patients — that is, periodically turning them onto their stomachs. Such positioning takes advantage of gravity to match areas of air-filled lung with areas of higher blood flow…
To read the entire article from The New Yorker, click https://www.newyorker.com/science/medical-dispatch/what-we-dont-know-about-covid-19